Classically, this type of external root resorption
occurs when infection is superimposed on a traumatic
injury – usually following replantation of an avulsed
tooth or a luxation injury. Nevertheless it can also be
induced in some cases of endodontic pathosis as shown
in Fig 15a. Despite the degree of external inflammatory
resorption, treatment can be successful (Fig 15b).
A prerequisite for external inflammatory root
resorption is damage to the normally protective
cementum/cementoid which then initiates surface
resorption exposing the underlying dentine to the
passage of bacteria or their metabolites from the root
canal to the external root surface. A normal
inflammatory response ensues including the activation
of clastic cells which results in resorption of both tooth
and bone. As the inflammatory response is chronic in
nature it is generally asymptomatic unless the infection
becomes acute, in which case the tooth will become
tender to touch and there may be the development of an
overlying swelling.
Radiographically external inflammatory root
resorption can be recognized by bowl-like radiolucencies
in both the tooth root and the adjacent bone. This is a
progressive form of root resorption which will
ultimately result in tooth loss. However, in most
instances external inflammatory root resorption can be
stabilized with treatment. As with other forms of
infection induced resorption, treatment involves the
thorough debridement and preparation of the root
canal system. Irrigation is a most important component
of this debridement process and the sequential use of
17% EDTAC, 1% sodium hypochlorite and a final
rinse with EDTAC solution has been shown to be a
most effective regimen resulting in a dentine surface
devoid of smear layer.
Such dentine preparation
facilitates the diffusion of medicaments such as
Ledermix paste through dentine to the external root
surface where the corticosteroid and antibiotic
components of the paste can exert a positive effect on the
clastic cells responsible for the resorptive processes.
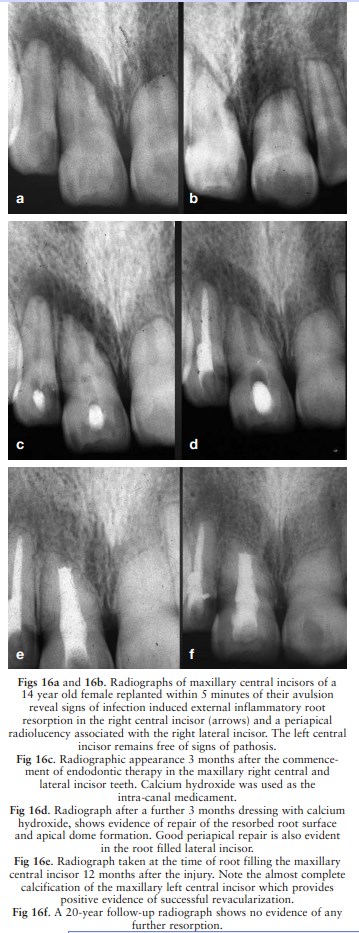
Calcium hydroxide has been widely used in the treat-ment
of external inflammatory root resorption
as illustrated in a case of external inflammatory root
An alternative approach involves the use of Ledermix
paste as the initial intra-canal medicament to act as an
anti-clastic agent. This root canal medication is
replaced at six-weekly intervals for a period of
approximately three months and then if there has been
radiographic signs of resorption control, calcium
hydroxide can be used to influence hard tissue
deposition on resorbed root surfaces. This sequential use
is shown in Figs 17a-17d which involved a case of
external inflammatory resorption observed six months
following the replantation of an incompletely developed
central incisor. A 10-year follow-up radiograph is
shown in Fig 17e.
Prevention of inflammatory root resorption: A tooth
with complete root development which has been
injury should, after replantation or repositioning, have
the pulp removed as soon as possible and the canal
dressed with Ledermix paste so that its anti-clastic
effect can be exerted in the early phases of the healing
process.
If calcium hydroxide is to be used as the
initial dressing material, treatment should be delayed
for at least two weeks to avoid cellular necrosis and
ankylosis.
In a tooth with an immature apex, with a
diameter greater than 2mm, there is a chance of
revascularization in all the above injuries, provided in
the case of a replanted tooth that the extra-oral period
is relatively short (30 minutes) or the tooth has been
stored in a medium which maintains the viability of the
periodontal ligament. Teeth with wide apices subjected
to such trauma should be monitored carefully at
monthly intervals for three months and at longer
intervals thereafter. If radiographic signs of
inflammatory root resorption become evident,
immediate endodontic intervention is required.