Any instrument which is placed in the root canal should be sterile, for two reasons. Firstly, to prevent the introduction to the root canal system of extraneous microorganisms, which may severely compromise treatment, for example pseudomonas.
Secondly, if instruments and devices were to be used on different patients, to prevent cross-infection between patients. Bacteria, viruses, fungi and prions may contaminate instruments and research has shown that some of these may not be destroyed by any method of sterilization.
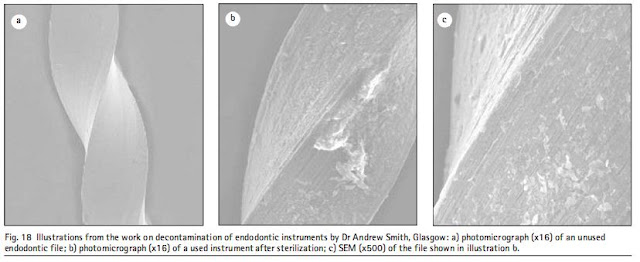
Figure 18 illustrates this dramatically. Concern has been raised over the sterilization of other items of dental equipment as well.
Under the Medical Devices Directive, the manufacturer of any dental instrument has an obligation to inform the end-user (ie the dentist) how their product should be decontaminated. It is essential that this guidance is followed. Whatever may be written in this and other texts may be superseded at any time. Dentists should therefore ensure that they are familiar with and conform to the manufacturer s instructions. At present, some endodontic instruments are marked with the symbol shown in Figure 19 indicating that they are single use instruments. It is assumed that all manufacturers will shortly follow this Medical Devices Directive. It may, however, be necessary to sterilize instruments for further treatment of the same patient on a subsequent occasion when crossinfection control would not be a problem. After use, instruments must be cleaned as soon as possible to remove debris which harbours and protects microorganisms. Cleaning is carried out by scrubbing in warm water and detergent, although the debris may be first removed from most root canal instruments by stabbing them into a sponge. The best method of cleaning is to place the instruments into an ultrasonic bath. The cavitational effects of ultrasonics will dislodge debris from places which are inaccessible to normal cleaning. When the instruments are clean they must be sterilized in an autoclave. Microorganisms are destroyed at lower temperatures and in a shorter period in moist heat as all biological reactions are catalysed in water. The disadvantages of autoclaving are that metal instruments tend to corrode and sharp instruments are dulled.
Secondly, if instruments and devices were to be used on different patients, to prevent cross-infection between patients. Bacteria, viruses, fungi and prions may contaminate instruments and research has shown that some of these may not be destroyed by any method of sterilization.
Figure 18 illustrates this dramatically. Concern has been raised over the sterilization of other items of dental equipment as well.
Under the Medical Devices Directive, the manufacturer of any dental instrument has an obligation to inform the end-user (ie the dentist) how their product should be decontaminated. It is essential that this guidance is followed. Whatever may be written in this and other texts may be superseded at any time. Dentists should therefore ensure that they are familiar with and conform to the manufacturer s instructions. At present, some endodontic instruments are marked with the symbol shown in Figure 19 indicating that they are single use instruments. It is assumed that all manufacturers will shortly follow this Medical Devices Directive. It may, however, be necessary to sterilize instruments for further treatment of the same patient on a subsequent occasion when crossinfection control would not be a problem. After use, instruments must be cleaned as soon as possible to remove debris which harbours and protects microorganisms. Cleaning is carried out by scrubbing in warm water and detergent, although the debris may be first removed from most root canal instruments by stabbing them into a sponge. The best method of cleaning is to place the instruments into an ultrasonic bath. The cavitational effects of ultrasonics will dislodge debris from places which are inaccessible to normal cleaning. When the instruments are clean they must be sterilized in an autoclave. Microorganisms are destroyed at lower temperatures and in a shorter period in moist heat as all biological reactions are catalysed in water. The disadvantages of autoclaving are that metal instruments tend to corrode and sharp instruments are dulled.